As iron continues to build up in the body, complications happen more often.5
60-70%
of deaths in thalassaemia major patients are due to cardiac disease and complications7
Causes of death in thalassaemia patients until the late 1990s7
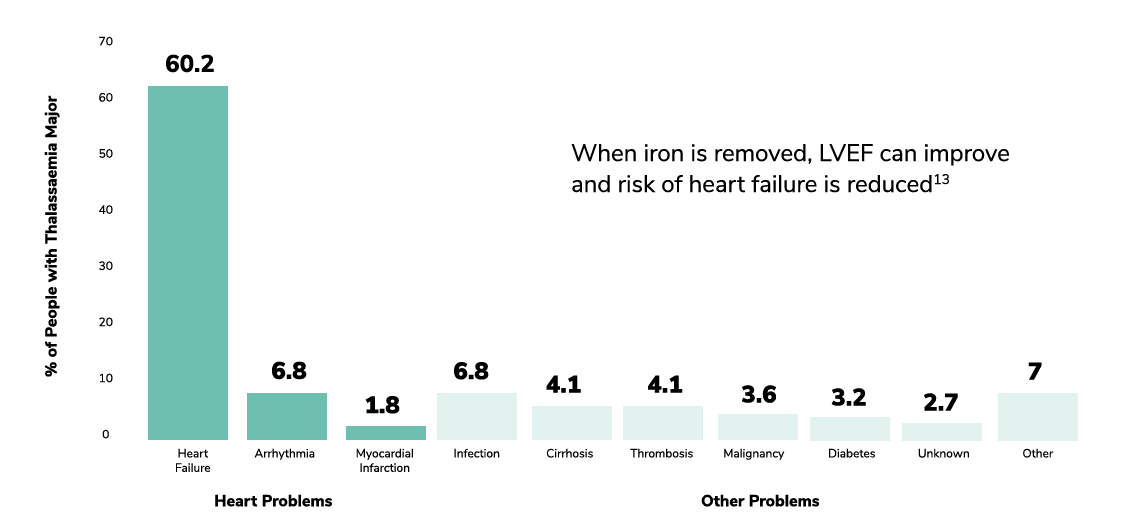
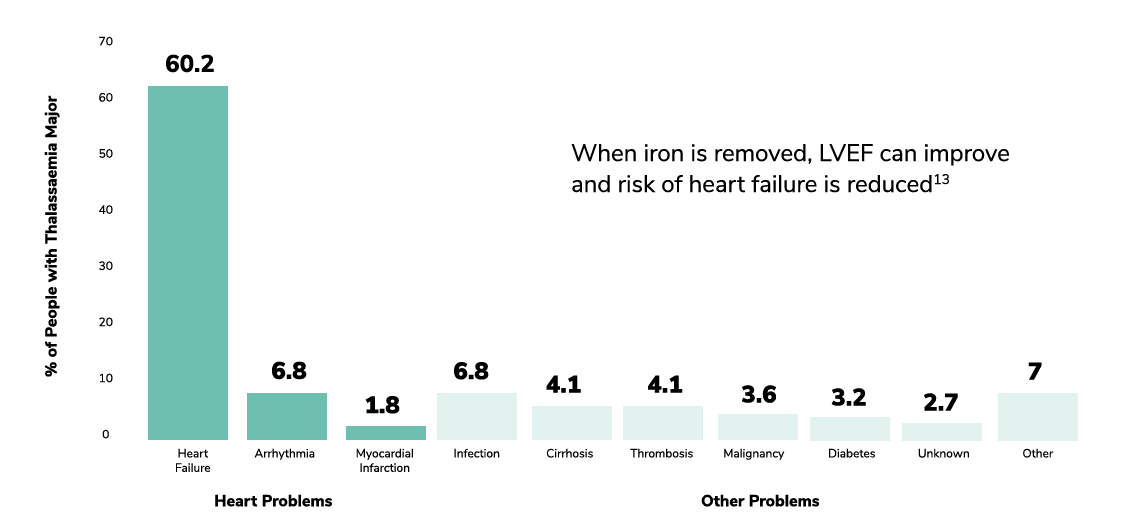
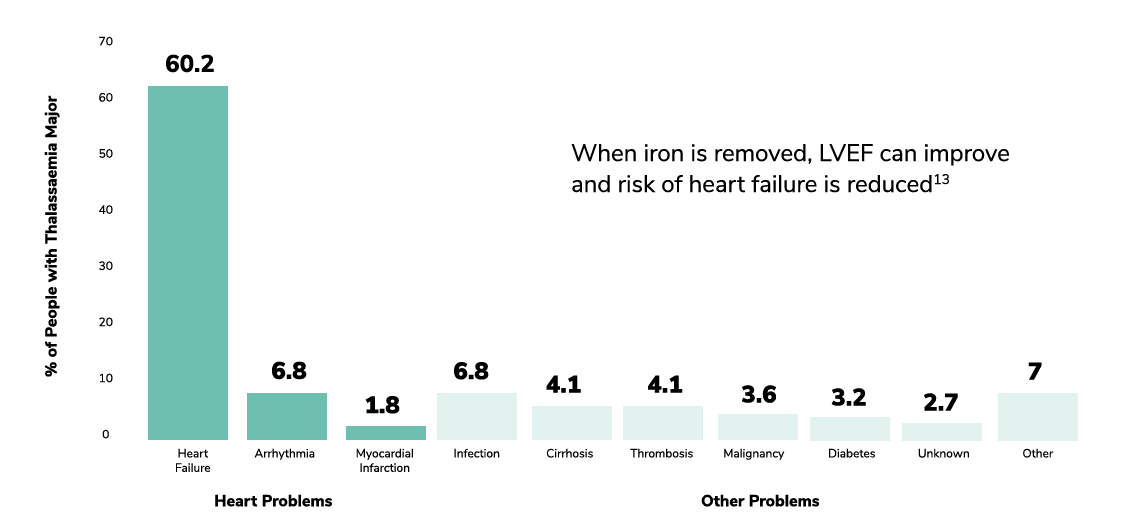
Adapted from Borgna-Pignatti C. et al. Haematologica 2004. Table 1, Causes of death for the entire population of patients and for those born after 1970; p. 1189
Monitor for renal/hepatic toxicity
Regular monitoring of both renal and hepatic toxicity can help optimise chelation and ensure patients are on an appropriate chelator.5
Chelation therapy needs to be individually tailored for each patient to respect their lifestyle and to minimise toxicity.5
Iron chelation needs to be adjusted regularly or even switched depending on iron level, weight, and tolerance to side effects.10
| Thalassaemia treatment guidelines support regular monitoring of serum ferritin, and cardiac and liver MRI T2*.10,14 | ||
|---|---|---|
| Parameter | Target | Recommended monitoring |
| Serum ferritin | <1,000 ng/mL | Monthly |
| Cardiac MRI T2* | 20 ms or higher | Annually (Or every 6 months for those patients with T2* <10 ms) |
| Liver iron concentration (LIC) | <3,000 µg/g dry weight | Annually |
*Frequency of monitoring and reference values may differ depending on country of practice. Please refer to your local guidelines.
Lowering serum ferritin and liver iron concentration are not enough5
For HCP: In case you want to report an adverse drug reaction you become aware of, please report it to your Health Authority according to the requirements set by the pharmacovigilance legislation.